Abstract
Enzalutamide is an oral androgen receptor signaling inhibitor utilized in the treatment of men with prostate cancer. It is a moderate inducer of the cytochrome P450 (CYP) enzymes CYP2C9 and CYP2C19, and a strong inducer of CYP3A4. It was also shown to be a mild inhibitor of the efflux transporter P-glycoprotein in patients with prostate cancer. Enzalutamide is primarily metabolized by CYP3A4 and CYP2C8. The risk of enzalutamide drug interactions arises primarily when it is coadministered with other drugs that interact with these CYPs, including CYP3A4. In this review, we begin by providing an overview of enzalutamide including its dosing, use in special populations, pharmacokinetics, changes to its prescribing information, and potential for interaction with coadministered drugs. Enzalutamide interactions with drugs from a wide range of medication classes commonly prescribed to patients with prostate cancer are described, including oral androgen deprivation therapy, agents used to treat a range of cardiovascular diseases, antidiabetic drugs, antidepressants, anti-seizure medications, common urology medications, analgesics, proton pump inhibitors, immunosuppressants, and antigout drugs. Enzalutamide interactions with common vitamins and supplements are also briefly discussed. This review provides a resource for healthcare practitioners and patients that will help provide a basis for the understanding and management of enzalutamide drug–drug interactions to inform decision making, improve patient safety, and optimize drug efficacy.
Plain Language Summary
Enzalutamide is a drug that is used to treat various stages of advanced prostate cancer, a type of cancer that begins in the prostate and may spread beyond the prostate. Enzalutamide stops testosterone from stimulating prostate cancer growth. Like other drugs, enzalutamide enters the bloodstream, and then is processed and removed from the body. Sometimes, when a person takes multiple drugs, one drug can make it difficult for the body to process and remove one or more of the other drugs. This is referred to as a drug interaction. Enzalutamide drug interactions can cause the level of other drugs in the body to increase or decrease in an abnormal way. It is also possible for certain other drugs to alter the levels of enzalutamide. Drug interactions that cause the level of a drug to get too low can prevent that drug from working effectively, whereas drug interactions that cause the level of a drug to get too high can lead to side effects of that drug. People with prostate cancer are mostly aged 65 years or older and often take medications to treat a variety of diseases. Examples include medications to treat heart conditions, diabetes, high cholesterol, high blood pressure, and many other conditions. Here, we describe enzalutamide drug interactions with these types of medications. Our goal is to provide a resource to help healthcare providers and patients better understand enzalutamide drug interactions and how to manage them to improve patient safety and drug effectiveness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Enzalutamide is a beneficial drug for the treatment of certain types of prostate cancer but requires management of potentially significant drug interactions. |
Most drug interactions stem from the fact that enzalutamide is a strong inducer of CYP3A4, a hepatic cytochrome P450 enzyme that is responsible for the metabolism of many other drugs on the market. |
Based on the current understanding of enzalutamide drug interactions, nearly all of them can be effectively managed with appropriate knowledge of which drugs pose interaction risks, when dose adjustments are indicated, and when alternative drugs can be substituted. |
1 Introduction
After lung cancer, prostate cancer was the second most diagnosed cancer in men in 2020 with an estimated 1.4 million new cases and 375,000 deaths worldwide [1]. The estimated number of new prostate cancer cases in the USA in 2023 is approximately 300,000 with 35,000 deaths [2]. Age is a risk factor for the onset of prostate cancer [3], and the median age at diagnosis is 67 years [2]. Men over 65 years of age commonly have other age-related comorbidities in addition to prostate cancer and the likelihood that prostate cancer will be associated with more comorbidities increases with increasing age at diagnosis [4].
Because older patients frequently have multiple health conditions, they are often prescribed many drugs in what is referred to as “polypharmacy” [5]. The presence of many coadministered medications puts patients at heightened risk for drug–drug interactions (DDIs) [5]. Therefore, it is critical to check for potential DDIs when prostate cancer drugs are given with other agents used to treat comorbidities. The goal of this review is to provide a resource to healthcare providers to improve their understanding of DDIs for the prostate cancer drug enzalutamide and enable them to make informed treatment decisions. Clinically, this is important as DDIs between enzalutamide and certain other medicines may result in a loss of efficacy of the coadministered drug or an increased risk of drug-related adverse effects [6,7,8].
In this review, we first provide a brief background describing types of DDIs and the roles of cytochrome P450 (CYP) enzymes and drug transporters in regulating plasma drug concentrations. We then describe enzalutamide, including its dosing, use in special populations, pharmacokinetics, changes to its prescribing information, and the basis for its potential interactions with coadministered drugs. Finally, the focus of the review is on describing DDIs between enzalutamide and other drugs commonly prescribed to patients with prostate cancer. Where data are available, we also briefly describe potential interactions between enzalutamide and commonly used vitamins and herbal supplements.
We did not use a strict a priori method for the literature search in this review. Instead, we generated a list of drugs and drug classes to consider for enzalutamide DDIs based on the authors’ input and clinical expertise. This list was based on the most common drugs utilized by the population of patients who are receiving prostate cancer therapy, i.e., those who are male, elderly, and with common comorbidities including heart disease and diabetes. Descriptions of individual DDIs, including a more detailed description of specific cases, relied on information obtained from multiple sources including drug prescribing information, Drugs.com [9], UpToDate (Lexicomp) [10], the Prescriber’s Digital Reference [11], literature sources identified via PubMed and Google Scholar searches using the drug names and classes in Table 1 as search terms, and the individual and collective expertise of the authors.
2 Molecular and Physiologic Basis for Drug–Drug Interactions (DDIs)
2.1 Types of DDIs
DDIs include pharmacokinetic and pharmacodynamic interactions [12] (Table 2). Pharmacokinetic interactions primarily consist of metabolic interactions involving CYP enzymes and include drug–transporter interactions, plasma protein DDIs, and absorptive DDIs [12]. Pharmacodynamic interactions typically consist of additive effects of two associated drugs [12]. DDIs may also impact the metabolic conversion of prodrugs, which are inactive drug precursors, to their active metabolites [13, 14].
2.2 Cytochrome P450 (CYP) Enzymes
Human CYP enzymes are the major enzymes responsible for drug metabolism and account for ~75% of drugs processed by enzymes [15]. CYP enzymes increase the hydrophilicity of compounds to aid in their excretion from the body and CYP-mediated drug metabolism plays a critical role in determining treatment outcomes by influencing drug action, safety, bioavailability, and resistance [15]. CYPs also convert certain prodrugs to their active metabolites [15]. The activity and expression levels of individual CYPs can vary significantly among individuals because of genetic differences [16, 17] and this is important to keep in mind when monitoring DDIs, as patients may not respond to drugs in the predicted manner. CYPs are mainly expressed in the liver, but also in the kidney, placenta, adrenal gland, gastrointestinal tract, and skin [15]. Approximately 80% of clinical drugs are metabolized by members of the CYP1, CYP2, and CYP3 families [18, 19]. CYP enzyme induction results from an increase in the amount of CYP enzymes and/or CYP enzymatic activity. CYP induction may in turn result in altered drug metabolism, such that the drug effect may be either decreased or remain unchanged. Conversely, CYP enzyme inhibition results from a decrease in CYP enzymatic activity. CYP inhibition may result in decreased drug metabolism and potentially increased drug concentration.
2.3 Drug Transporters: P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP)
Membrane transporters play key roles in the pharmacokinetics, safety, and efficacy of drugs [20]. These include P-gp (also known as multidrug resistance 1 [MDR1]), BCRP (also known as ABCG2), organic cation transporters (OCTs), organic anion transporters (OATs), and organic anion transporting polypeptides (OATPs) [20]. P-gp and BCRP are major transporters that regulate absorption, disposition, and excretion of many drugs and play key roles in DDIs [20, 21]. P-gp is expressed in the small intestine, kidney, liver, and brain endothelium [20] where it plays a role in the blood–brain barrier (BBB) in limiting entry of various drugs into the central nervous system [20]. P-gp is also involved in intestinal absorption and intestinal, biliary, and urinary excretion of drugs [20]. BCRP is expressed in the gastrointestinal tract, liver, kidney, brain endothelium, mammary tissue, testes, and placenta [20]. BCRP limits oral bioavailability and the transport of some substrates across the BBB, blood–testes barrier, and maternal–fetal barrier [20]. P-gp/BCRP enzyme induction results from an increase in the amount of P-gp/BCRP enzymes and/or the enzymatic activity of P-gp/BCRP [21], and both transporters are transcriptionally regulated by the pregnane xenobiotic receptor (PXR) [21,22,23]. Drug-induced activation of PXR and subsequent induction of drug-metabolizing enzymes and transporters are central mechanisms driving DDIs [24]. Decreased drug absorption and decreased drug concentration following P-gp/BCRP induction can result in the drug effect being either decreased or remaining unchanged. Conversely, P-gp/BCRP enzyme inhibition resulting from a decrease in P-gp/BCRP transporter activity has the potential to cause DDIs.
3 Enzalutamide
Enzalutamide is a nonsteroidal androgen receptor signaling inhibitor indicated for the treatment of men with advanced metastatic hormone-sensitive prostate cancer (HSPC) and castration-resistant prostate cancer (CRPC) [25,26,27,28], as well as nonmetastatic castration-sensitive prostate cancer with biochemical recurrence at high risk of metastasis [29].
3.1 Dosing
Enzalutamide is administered once-daily via oral dosing (160 mg) [6, 30, 31]. Patients receiving enzalutamide for advanced prostate cancer (HSPC and CRPC) should be undergoing testosterone suppression, i.e., they should be receiving a gonadotropin-releasing hormone (GnRH) analog concurrently or should have had a bilateral orchiectomy [26].
3.2 Pharmacokinetics
The median time to peak drug concentration (Tmax) of enzalutamide is 1 hour following a single 160 mg dose of capsules and 2 hours following a single 160 mg dose of tablets [32]. The mean volume of distribution is 110 L (29%) after a single oral dose [32]. Enzalutamide is 97–98% bound to plasma proteins, primarily albumin, and its active metabolite, N-desmethyl enzalutamide, is 95% bound to plasma proteins [6]. Enzalutamide is primarily metabolized by CYP3A4 and CYP2C8 to form the active metabolite N-desmethyl enzalutamide and an inactive carboxylic acid metabolite [33]. Clinical DDI studies evaluating the effect of a strong CYP2C8 and a strong CYP3A4 inhibitor on the combined pharmacokinetics of enzalutamide and N-desmethyl enzalutamide and the effect of enzalutamide on the pharmacokinetics of oral dose-sensitive substrates for CYP2C8, CYP2C9, CYP2C19, or CYP3A4 have indicated that enzalutamide is a moderate inducer of CYP2C9 and CYP2C19, and a strong inducer of CYP3A4 [33]. The mean terminal half-life (t1/2) for enzalutamide after a single oral dose is 5.8 days (2.8–10.2 days); enzalutamide achieves steady state 28 days following administration [32]. The mean t1/2 for N-desmethyl enzalutamide after a single oral dose is approximately 7.8–8.6 days [32]. Enzalutamide is primarily eliminated by hepatic metabolism [32].
3.3 Clinical Study: Interactions with P-gp and BCRP
In vitro DDI studies have indicated that enzalutamide is an inhibitor of P-gp and BCRP [34], and it has been suggested to have the potential for transporter-mediated DDIs via interactions with P-gp and BCRP when coadministered to patients with medications that are substrates of these efflux transporters [35]. In addition, enzalutamide could potentially induce P-gp and BCRP as it is a strong inducer of CYP3A4 and because both transporters and CYP3A4 are induced by PXR [22, 24, 36]. To test the effects of enzalutamide on P-gp and BCRP, a phase I, open-label, placebo-controlled, fixed-sequence, crossover DDI study was conducted in men with metastatic CRPC [35]. The objective of this study was to measure the effects of enzalutamide on the pharmacokinetics of a transporter-probe cocktail containing the P-gp and BCRP substrates, digoxin and rosuvastatin [35]. Concomitant administration of enzalutamide with the P-gp substrate digoxin resulted in increased digoxin exposure (area under the curve [AUC] and plasma maximum concentration [Cmax] of digoxin increased by 33% and 17%, respectively), suggesting that enzalutamide is a “mild” inhibitor of P-gp [35]. No pharmacokinetic interactions were observed between enzalutamide and rosuvastatin, suggesting that enzalutamide had no effect on BCRP in the men studied [35]. The authors concluded that enzalutamide-mediated induction of CYP2C9, CYP2C19, and CYP3A4 does not necessarily predict the overall effect on P-gp and BCRP, and that concomitant administration of enzalutamide with medications that are P-gp and BCRP substrates may not require dose adjustment [35]. The US prescribing information for enzalutamide was updated in September 2022 based on the results of this study [6].
3.4 Use of Enzalutamide in Special Populations
No overall differences in safety and effectiveness have been observed between patients aged <75 years and those aged ≥75 years treated with enzalutamide in clinical trials [37, 38]. No dosage modification is required in patients with mild-to-moderate renal impairment. Of note, enzalutamide has not been studied in severe/end-stage renal disease [32]. No dosage modification is required in mild, moderate, or severe hepatic impairment [6].
3.5 Enzalutamide and DDIs
More than 50% of older men with prostate cancer have one or more chronic comorbid conditions [39]. Polypharmacy is prevalent among elderly patients [5] and DDIs are an important consideration for clinical use of enzalutamide [6].
Enzalutamide reduced plasma exposure to drugs that are substrates of CYP2C9, CYP2C19, and especially CYP3A4 at steady state [6, 33]. Examples of drugs with concentrations reduced by enzalutamide include midazolam, warfarin, and omeprazole [33] (Fig. 1A). Specifically, enzalutamide decreased the AUC for midazolam by 86%, for warfarin by 56%, and for omeprazole by 72%. In general, coadministration of enzalutamide should be avoided with CYP3A4, CYP2C9, or CYP2C19 substrates for which a minimal decrease in concentration may lead to therapeutic failure of the substrate [33]. It is possible for enzalutamide to have DDIs that do not cause meaningful clinical outcomes [40]. For example, enzalutamide may decrease the plasma concentration of a coadministered drug without decreasing the efficacy of that drug. Alternatively, enzalutamide may increase the exposure of a coadministered drug without affecting the adverse event profile of that drug. These scenarios are more likely when enzalutamide is coadministered with drugs that have a high therapeutic index. Risks of adverse events due to DDIs are primarily associated with narrow therapeutic index drugs for which a small change in the enzalutamide concentration could have a meaningful clinical outcome [33].
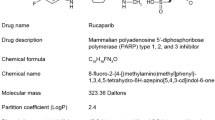
Enzalutamide clinical drug interaction studies. Enzalutamide is metabolized by CYP2C8 and CYP3A4. Enzalutamide is a strong CYP3A4 inducer and a moderate CYP2C9 and CYP2C19 inducer. Enzalutamide was shown to be a mild inhibitor of human P-gp. AUC area under the curve (systemic drug exposure), Cmax maximum concentration after a single dose, CYP cytochrome P450, P-gp P-glycoprotein, PI prescribing information
Coadministered drugs can also impact the concentration of enzalutamide and its active metabolite N-desmethyl enzalutamide. Enzalutamide is metabolized by CYP2C8 and CYP3A4 [33]; therefore, coadministration of enzalutamide with drugs that either induce or inhibit these enzymes can alter enzalutamide concentrations. Gemfibrozil is an example of a strong CYP2C8 inhibitor and rifampin is an example of a strong CYP3A4/moderate CYP2C8 inducer (Fig. 1B). Gemfibrozil increased the AUC of enzalutamide plus N-desmethyl enzalutamide by 2.2-fold, while rifampin decreased the AUC by 37%. To mitigate the risk to patients, it is recommended to avoid coadministration of enzalutamide with a strong CYP2C8 inhibitor. However, if coadministration is unavoidable, use enzalutamide 80 mg once daily during concomitant use with a strong CYP2C8 inhibitor [33]. The dose of enzalutamide should be increased to 240 mg once daily for patients taking strong CYP3A4 inducers [6]. Additional examples of strong CYP3A4 inducers in addition to rifampin include carbamazepine, phenobarbital, and phenytoin [41].
In summary, enzalutamide can decrease the concentration of coadministered drugs that are substrates of CYP3A4, CYP2C9, or CYP2C19. It can also increase the concentration of drugs, such as digoxin, that are substrates of P-gp. Furthermore, coadministration of enzalutamide with drugs that are strong CYP2C8 inhibitors can increase enzalutamide plasma concentrations, whereas coadministration of enzalutamide with drugs that are strong CYP3A4 inducers can result in decreased enzalutamide blood concentrations. Prescribers should refer to the prescribing information of the medications being administered concomitantly with enzalutamide to assess the need to adjust medication doses based on the degree of potential CYP or transporter effects. However, prescribing information may not always be sufficient to fully account for a DDI and its management. Indeed, DDIs with a new drug may not be included in the prescribing information until revision. Therefore, in addition to referring to drug interaction checkers such as those provided by Drugs.com and UpToDate (Lexicomp), it is also important to contact the pharmacovigilance unit and other specialists (e.g., cardiologists) to help identify and manage DDIs. In general, the combined expertise provided by multidisciplinary teams of physicians and other healthcare practitioners can substantially improve the management of complex treatment-related decisions and improve patient outcomes [42].
4 Enzalutamide with Specific Medication Classes
4.1 Patients With Prostate Cancer Are Commonly Treated for Various Comorbidities
Comorbidities that coexist in patients with prostate cancer over 65 years of age include hypertension, hypercholesterolemia, diabetes, cardiovascular diseases, chronic back pain, depression and anxiety, and others [43]. Therefore, patients with prostate cancer are commonly treated with drugs for a variety of other conditions and these need to be carefully managed together with medications aimed at treating their prostate cancer. Here, we describe potential DDIs between enzalutamide and other commonly prescribed drugs (Table 1) and frequently used supplements among patients with prostate cancer. We also propose strategies for preventing potentially problematic enzalutamide DDIs.
4.2 Oral Androgen Deprivation Therapy
Enzalutamide is prescribed in combination with androgen deprivation therapy (ADT) [26]. Commonly prescribed ADT drugs include the GnRH agonists leuprolide, goserelin, and triptorelin, and the GnRH antagonist degarelix [44]. These drugs are delivered via injection, are not metabolized via hepatic CYPs, and are not predicted to interact with enzalutamide [9]. Relugolix is an orally administered GnRH antagonist ADT that suppresses testosterone production in the treatment of prostate cancer [44]. Relugolix is a substrate of CYP3A, CYP2C8, and P-gp, and an inducer of CYP3A and CYP2B6 [45]. As enzalutamide is a mild P-gp inhibitor [35], it could increase the plasma concentration of P-gp substrates such as relugolix. However, enzalutamide is a strong inducer of CYP3A4, providing a mechanism through which it could potentially decrease the plasma concentration of relugolix. The HERO study demonstrated that relugolix suppresses testosterone in a manner superior to that of leuprolide in men with advanced prostate cancer [46]. In a subgroup and pharmacokinetic/pharmacodynamic analysis of the HERO study, George et al. demonstrated that treatment of patients with advanced prostate cancer with relugolix was associated with similar efficacy and safety outcomes with and without coadministration of enzalutamide [47]. Importantly, the results of this study suggest that any effects enzalutamide may have on relugolix metabolism do not have an overall impact on relugolix drug exposure or relugolix-mediated testosterone suppression [47]. Therefore, when enzalutamide is combined with relugolix, no dose adjustments are needed for either medication.
4.3 Enzalutamide and Agents Used to Treat Cardiovascular Diseases
Cardiovascular diseases are highly prevalent among patients with prostate cancer, especially those who are over 65 years of age [48]. Therefore, drugs used to treat and/or prevent cardiovascular disease will frequently need to be managed in patients over 65 years of age, including those with prostate cancer [49]. These include antithrombotic agents, statins, antihypertensive agents, antiarrhythmic agents, and drugs used to treat heart failure (HF).
4.3.1 Antithrombotic Agents
Anticoagulants and antiplatelet agents are critical for the prevention of thrombosis, which is the leading cause of all-cause death worldwide [50, 51]. However, a serious challenge posed by these drugs is the side effect of bleeding and this can be exacerbated by drug interactions.
4.3.1.1 Anticoagulants
Anticoagulant agents are primarily used for the treatment or prevention of venous or arterial thromboses [51]. They inhibit the coagulation cascade and thrombus formation by inhibiting factor Xa (FXa) or thrombin [51].
4.3.1.2 Direct Oral Anticoagulants
Direct oral anticoagulants (DOACs) are antithrombotic drugs that include apixaban, rivaroxaban, edoxaban, and dabigatran (Fig. 2). Apixaban, rivaroxaban, and edoxaban inhibit FXa, whereas dabigatran inhibits thrombin [51]. Apixaban and rivaroxaban are subject to potential DDIs by dual inhibitors and inducers of CYP3A4 and P-gp [52]. The effect of enzalutamide on the plasma concentration of these drugs is unclear because of opposing CYP3A4 and P-gp interactions. However, as enzalutamide is a strong CYP3A4 inducer and a mild P-gp inhibitor, its effects on CYP3A4 may be expected to be predominant resulting in a potential decrease in apixaban and rivaroxaban plasma concentrations, and therapy modification should be considered. Otsuka et al. [53] integrated in vitro and in vivo data into a physiologically based pharmacokinetic model to predict the extent to which enzalutamide and its active metabolite, N-desmethyl enzalutamide, impact apixaban and rivaroxaban plasma concentrations. The results predicted a 31% decrease in AUC and no change in Cmax for apixaban and a 45% decrease in AUC and a 25% decrease in Cmax for rivaroxaban following coadministration of the clinically relevant dose of 160 mg of enzalutamide [53]. Based on this study and current prescribing information, coadministration of these DOACs with enzalutamide should be carefully monitored with possible changes to dosing as necessary to ensure that drug efficacy and safety are maintained. Dabigatran and edoxaban are only minimally metabolized by CYPs and are only subject to DDIs by inhibitors and inducers of P-gp [52]. As enzalutamide was reported to be only a mild inhibitor of P-gp in human studies [35], any potential for DDIs with dabigatran and edoxaban may be less than for apixaban and rivaroxaban. However, concomitant use of P-gp inhibitors in renally impaired patients can increase the exposure of dabigatran, in which case the dabigatran dose should be reduced or coadministration should be avoided [54]. Dosing of dabigatran with enzalutamide should be based on the indication and level of renal dysfunction and we recommend that a pharmacist should be consulted to assist with the appropriate dose reduction of dabigatran or to determine if use of another DOAC is warranted.
4.3.1.3 Warfarin
Warfarin is a vitamin K antagonist that blocks the coagulation cascade and thrombus formation by inhibiting thrombin [51]. Warfarin is a narrow therapeutic index medication that is a substrate of CYP2C9 and CYP3A4 [55]. As enzalutamide is a strong CYP3A4 inducer and moderate CYP2C9 inducer, it also has the potential to decrease the effect of warfarin (decrease international normalized ratio [INR]) by decreasing the exposure of warfarin. Coadministration of enzalutamide and warfarin should be avoided if possible or additional INR monitoring should be conducted if coadministration of these two drugs is unavoidable (Fig. 2).
4.3.1.4 Antiplatelet Agents
Antiplatelet agents primarily prevent arterial thrombus formation by disrupting the platelet cascade [51].
4.3.1.5 P2Y12 Inhibitors
Clopidogrel, prasugrel, and ticagrelor inhibit platelet activation by blocking platelet P2Y12 adenosine receptors [51]. These agents are commonly used to protect against strokes and heart attacks [56]. They also play an important role together with aspirin in dual antiplatelet therapy (DAPT) after coronary stent placement to prevent stent thrombosis/restenosis [57,58,59]. Although DAPT has proven to be successful in preventing stent thrombosis/restenosis, the benefits of prolonged DAPT must be carefully balanced against an increased bleeding risk [60]. Notably, it is important for patients to coordinate changes in DAPT with their cardiologist as switching between different P2Y12 inhibitors can be challenging because of their different potencies, half-lives, and the need for specific and appropriate loading doses [61]. If not done correctly, these changes can result in stent thrombosis, which can be fatal.
Clopidogrel and ticagrelor have known interactions with enzalutamide (Fig. 2). Clopidogrel is a prodrug that relies on CYP2C19 for conversion to its active metabolite [14] (Fig. 3). Clopidogrel is also converted to an inactive acyl-β-glucuronide metabolite that is a time-dependent inhibitor of CYP2C8 [62]. Clopidogrel interacts with enzalutamide via two distinct mechanisms (Fig. 3): (1) enzalutamide can induce CYP2C19 and therefore has the potential to increase serum exposure to the active metabolite of clopidogrel; (2) as CYP2C8 is the primary enzyme responsible for metabolizing enzalutamide, clopidogrel has the potential to increase enzalutamide exposure. Because the inactive metabolite of clopidogrel is a strong CYP2C8 inhibitor, the prescribing information for clopidogrel recommends a dose adjustment and appropriate monitoring of drugs that are primarily cleared by CYP2C8 [63]. The prescribing information for enzalutamide also states that it should not be coadministered with strong CYP2C8 inhibitors [6]. However, in gauging the real effect of CYP2C19 induction on the amount of active metabolite formed, it is important to note that only ~15% of clopidogrel is converted to its active metabolite [14], and dose adjustments are not provided for enzalutamide for use with moderate CYP2C8 inhibitors [6]. In summary, coadministration of clopidogrel and enzalutamide should be carefully considered and if both drugs are coadministered, patients should be carefully monitored for increased pharmacologic effects of both medications. Ticagrelor is primarily metabolized via CYP3A4 and its plasma concentration may be reduced upon coadministration with strong CYP3A4 inducers [64], such as enzalutamide. Coadministration of ticagrelor with strong CYP3A4 inducers, such as enzalutamide, may reduce the exposure and efficacy of ticagrelor and should be avoided [64]. In contrast to clopidogrel and ticagrelor, prasugrel is only a minor substrate of CYP3A4 and has no known interactions with enzalutamide [9] (Fig. 2).
4.3.1.6 Aspirin
Aspirin (ASA) is an irreversible inhibitor of cyclo-oxygenase 1 that reduces the production of thromboxane within platelets, thereby inhibiting platelet aggregation and thrombus formation. Low-dose ASA (81 mg/day) can be effective at preventing heart attacks and strokes [65]. In addition to its role in DAPT, mentioned above, most clinicians consider ASA to be critical for secondary prevention of myocardial infarction (MI) and atherosclerotic cardiovascular disease [66]; many patients with prostate cancer will have already had either stroke, MI, or coronary artery disease (CAD), which warrant ASA treatment. Fortunately, ASA does not have known interactions with enzalutamide [9] (Fig. 2).
4.3.2 Statins
Statins are 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors used for the treatment of hypercholesterolemia, with high efficacy in reducing plasma low-density lipoprotein (LDL) and triglyceride levels [67]. Atorvastatin is a substrate of CYP3A4 and the transporters P-gp and BCRP [68], whereas simvastatin [69] and lovastatin [70] are primarily substrates of CYP3A4. Therefore, each of these drugs has potential for an interaction with enzalutamide [9]. Fluvastatin is primarily metabolized by CYP2C9 [71]. As enzalutamide is a moderate inducer of CYP2C9, it can also potentially interact with fluvastatin [9] with the potential to reduce fluvastatin exposure. Therefore, liver function and lipid levels should be monitored when statins are coadministered with enzalutamide to assess the safety and efficacy of statins. This should include checking a patient’s lipid panel at baseline before starting statin therapy or adjusting statin dosage levels during therapy and conducting additional monitoring every 6–8 weeks to assess the treatment response. If lipid control is satisfactory with no evidence of adverse events, subsequent lipid monitoring can be conducted every 4–6 months [72]. However, atorvastatin (revised 11/2021), simvastatin (revised 05/2022), and fluvastatin (revised 10/2012) product recommendations do not preclude coadministration or provide dose adjustment recommendations [68, 69, 71]. The BCRP substrates, pitavastatin, pravastatin, and rosuvastatin, are preferred statins for patients who take enzalutamide as these statins are minimally metabolized by CYPs [73] and either have a moderate or no known basis for interaction with enzalutamide [9]. Of these three statins, rosuvastatin should be emphasized in particular as it is also a high-intensity statin and was shown to reduce LDL levels to a greater extent than atorvastatin, simvastatin, and pravastatin [74]. At the highest dose of 40 mg, rosuvastatin reduced LDL levels by 55% compared with 51% for atorvastatin 80 mg and 46% pravastatin 80 mg [74].
4.3.3 Antihypertensive Agents
Calcium (Ca) channel blockers (e.g., amlodipine, diltiazem, verapamil, and others) are frequently prescribed to decrease blood pressure in patients with hypertension [75]. Most Ca channel blockers are metabolized by CYP3A4 [76]. As enzalutamide is a potent inducer of CYP3A4 [6, 33], there is a potential for a DDI where enzalutamide may decrease the plasma concentrations of many Ca channel blockers [6, 33]. Concomitant use of Ca channel blockers, such as amlodipine, with strong CYP3A4 inducers, such as enzalutamide, should be carefully considered [77]. If coadministration is necessary, the pharmacologic response of the Ca channel blocker should be monitored closely following the initiation or discontinuation of enzalutamide, and its dosage adjusted as necessary. If a patient requires treatment for hypertension, an angiotensin-converting enzyme (ACE) inhibitor, such as benazepril [78], which has no known interactions with enzalutamide [9], may be preferable to a Ca channel blocker. Beta-blockers, such as carvedilol, are also used to treat hypertension [79] and may also be preferable as they are not known to have interactions with enzalutamide [9].
4.3.4 Antiarrhythmic Agents
ADT has the potential to prolong the QT corrected for heart rate (QTc) interval and therefore the benefit–risk ratio of coadministration of enzalutamide with drugs known to prolong the QTc interval and/or induce Torsade de Pointes such as Class IA (e.g., disopyramide, quinidine, and procainamide) or Class III (e.g., amiodarone, dofetilide, and sotalol) antiarrhythmic agents [80] should be carefully considered [8]. However, in clinical practice, we only avoid prescribing enzalutamide if the patient has prolonged QTc or if the pharmacist raises a specific concern about a particular medication. In our opinion, potential risks of DDIs with enzalutamide and other drugs known to prolong the QTc interval can be safely overcome for most patients through multidisciplinary monitoring of serial electrocardiograms (EKGs) and ensuring that electrolytes are carefully managed. In this regard, we note that when the effects of enzalutamide 160 mg/day were evaluated in 796 men with CRPC, no large differences in the QTc interval caused by enzalutamide were observed [34]. Digoxin is a muscarinic M2 receptor activator Class IID antiarrhythmic drug [80] that is commonly prescribed for arrhythmia. As discussed above, digoxin is a P-gp substrate and coadministration of enzalutamide with digoxin increased digoxin exposure leading to the designation of enzalutamide as a mild P-gp inhibitor [35]. Poondru et al. concluded that dose modifications would most likely not be needed upon coadministration of enzalutamide and digoxin [35].
4.3.5 Other Heart Medications
Valsartan is an angiotensin type II receptor antagonist that blocks vasoconstriction [81]. Sacubitril is a prodrug that is activated to become a neprilysin inhibitor that reduces blood volume [82]. The combination of valsartan and sacubitril constitutes an important treatment for patients with heart failure [83]. These drugs do not have known interactions with enzalutamide [9]. Sodium-glucose cotransporter-2 (SGLT2) inhibitors are effective antidiabetic therapies, as discussed below, but also have significant cardiovascular benefits via mechanisms independent of improved glycemic control that are being intensively investigated [84]. SGLT2 inhibitors also do not have known interactions with enzalutamide (see below). Another important medication class in HF are mineralocorticoid receptor antagonists, which include spironolactone and eplerenone [85]. These drugs are both similarly effective in treating patients with congestive HF. However, eplerenone is primarily metabolized by CYP3A4 and it has been reported that St John’s Wort, a CYP3A4 inducer, may reduce eplerenone concentrations by 30% [85]. Therefore, while spironolactone and enzalutamide are not anticipated to have drug interactions, there is potential for an interaction between enzalutamide and eplerenone [9].
4.4 Antidiabetic Agents
Together with cardiovascular diseases, diabetes is highly prevalent among patients with prostate cancer over the age of 65 years [48]. Sulfonylureas, including glyburide, gliclazide, and glimepiride, are frequently used hypoglycemic agents for the treatment of type 2 diabetes [86, 87]. These antidiabetic drugs are primarily metabolized by CYP2C9 [87] and therefore, there may be potential for a DDI and susceptibility to reduced plasma concentrations upon coadministration with enzalutamide, a moderate CYP2C9 inducer. Dipeptidyl-peptidase 4 (DPP4) inhibitors, such as saxagliptin, are also used to treat type 2 diabetes [88]. Saxagliptin is primarily metabolized by CYP3A4/5 [88] and, therefore, there may be potential for a DDI and increased risk for reduced drug efficacy when coadministered with enzalutamide, a strong CYP3A4 inducer. One effective alternative to these drugs is metformin, a widely prescribed medication for type 2 diabetes with no known interactions with enzalutamide [9]. SGLT2 inhibitors are also effective in treating type 2 diabetes and, importantly, they are not metabolized by CYPs that are induced by enzalutamide [89] and are not known to have interactions with enzalutamide.
4.5 Antidepressants
Depression is common among elderly patients, particularly those with cancer [90]. Citalopram is a commonly prescribed serotonin-selective reuptake inhibitor (SSRI) antidepressant medication that can cause dose-dependent prolongation of the QTc interval [91]. Therefore, coadministration of ADT/enzalutamide together with citalopram should be carefully considered to avoid risk of prolonged QTc and Torsade de Pointes. However, as discussed above, it should be possible to overcome potential QTc issues in most patients through careful multidisciplinary monitoring of serial EKGs and ensuring that electrolytes are carefully managed. Fluoxetine and sertraline are additional SSRIs that can also lengthen the QTc interval but to a lesser degree than citalopram [92]. Therefore, these two drugs are predicted to have more moderate DDI risks with enzalutamide compared with citalopram [9].
Serotonin and norepinephrine reuptake inhibitors (SNRIs) (e.g., venlafaxine, desvenlafaxine, and duloxetine) may be preferable alternatives to SSRIs for the treatment of depression in patients with prostate cancer who are also being treated with enzalutamide, as SNRIs have a low risk for QTc prolongation [93, 94]. While venlafaxine can prolong the QTc interval and may pose a moderate risk when coadministered with enzalutamide, no significant risk of QTc prolongation was observed for duloxetine [94], and neither desvenlafaxine nor duloxetine have known interactions with enzalutamide [9].
4.6 Antiseizure Medications
Several antiseizure medications including carbamazepine, phenobarbital, phenytoin, and primidone (partially metabolized to phenobarbital) are potent CYP2C9 and/or 3A4 inducers [41]. As enzalutamide is metabolized by CYP3A4, there is potential for a DDI and plasma concentrations may be decreased if enzalutamide is coadministered with these drugs. Therefore, if concomitant use of enzalutamide and these drugs cannot be avoided the enzalutamide dosage should be increased from 160 mg to 240 mg once daily [6]. If the interacting antiseizure medication is discontinued, the original enzalutamide dose of 160 mg once daily can be re-established. Valproic acid, lamotrigine, gabapentin, and topiramate are alternative antiseizure medications that do not have known interactions with enzalutamide [9].
4.7 Common Urology Medicines
Oxybutynin is a commonly prescribed antimuscarinic agent that is used to treat overactive bladder (OAB) [95]. Because of its anticholinergic properties, oxybutynin should be used with caution in elderly patients owing to its potential negative effect on cognitive function [96]. Oxybutynin is primarily metabolized by CYP3A4 [97], which is strongly induced by enzalutamide. Therefore, there is potential for a DDI that may result in decreased plasma concentrations of oxybutynin if coadministered with enzalutamide. Mirabegron is also used to treat OAB [95] and may similarly interact with enzalutamide [9]. Trospium is a potentially preferable alternative to oxybutynin and mirabegron for the treatment of OAB as it has no known interactions with enzalutamide [9]. Tamsulosin is a commonly prescribed alpha adrenergic receptor blocker used to treat enlarged prostate and difficulty urinating [98]. Tamsulosin is also metabolized by CYP3A4 and therefore there is potential for a DDI if coadministered with enzalutamide, which may potentially cause reduced tamsulosin serum exposure [9].
4.8 Pain Medications
Enzalutamide coadministration with oxycodone, methadone, tramadol, and fentanyl may result in decreased plasma concentration of these opioid analgesics as they are primarily metabolized by CYP3A4 [99], which is strongly induced by enzalutamide. It was recently shown that enzalutamide decreases exposure to oxycodone and its active metabolite oxymorphone [100]. This interaction is clinically relevant as pain may not be adequately controlled when both drugs are present and there is a risk of overdose upon enzalutamide discontinuation [100]. Enzalutamide coadministration with these opioids should be monitored closely. In particular, the pharmacologic response to the opioid should be checked regularly when enzalutamide is added to or withdrawn from therapy, and the opioid dosage should be adjusted as necessary. Morphine, hydromorphone, and oxymorphone are preferable alternatives as they are not metabolized by CYPs [99] and have no known interactions with enzalutamide [9].
4.9 Proton Pump Inhibitors (PPIs)
PPIs inhibit stomach acid production and treat common acid-related disorders including heartburn, ulcers, and gastroesophageal reflux disease [101]. There are currently six PPIs available: omeprazole, esomeprazole, lansoprazole, dexlansoprazole, rabeprazole, and pantoprazole [101]. Omeprazole, esomeprazole, lansoprazole, and rabeprazole are primarily metabolized by CYP2C19, whereas dexlansoprazole and pantoprazole are metabolized by CYP2C19 and CYP3A4 [101]. Coadministration of enzalutamide 160 mg once daily with omeprazole decreased omeprazole AUC by 70% and Cmax by 62% [6] (Fig. 1A). However, product recommendations do not preclude coadministration or provide dose-adjustment recommendations [102] and clinical discretion is advised. Dexlansoprazole, which is the R-enantiomer of lansoprazole, is a highly efficacious delayed-release PPI with safety and side-effect profiles that are similar to lansoprazole [103]. Dexlansoprazole is the preferred PPI for coadministration with enzalutamide as it has no known drug interactions, whereas the other five available PPIs have the potential for moderate interactions [9]. Notably, the solubility of enzalutamide is not affected by pH over the physiological range [32] and, therefore, PPIs are not expected to alter enzalutamide absorption.
4.10 Immunosuppressants
Commonly used immunosuppressants include cyclosporine, tacrolimus, everolimus, and sirolimus [104]. Cyclosporine can inhibit CYPs that metabolize enzalutamide and, therefore, it has the potential to increase the plasma concentration of enzalutamide [9]. Tacrolimus, everolimus, and sirolimus are metabolized by CYP3A4 [104], and their plasma concentrations can be decreased by enzalutamide potentially resulting in a loss of clinical efficacy [9].
4.11 Antigout Drugs
Gout is an inflammatory disease caused by build-up of uric acid in joints. Painful flare-ups can be treated with colchicine, nonsteroidal anti-inflammatory drugs (NSAIDs; e.g., naproxen sodium), or prednisone, whereas uric acid accumulation can be ameliorated by treatment with allopurinol [105]. As colchicine and prednisone are metabolized by CYP3A4, and naproxen sodium is metabolized by CYP2C8 and CYP2C9, the plasma concentrations of each of these drugs have the potential to be decreased by enzalutamide [9]. No DDIs are predicted between enzalutamide and allopurinol [9].
4.11.1 Supplements
The use of complementary and alternative medicines is highly popular among patients with cancer. It is estimated that approximately three quarters of patients with cancer who use alternative medicines in addition to their conventional cancer therapies do not inform their treating physician [106]. One of the best characterized examples of an alternative medicine with clinically significant drug interactions is St. John’s Wort, which is used to treat mild-to-moderate depression [106]. St John’s Wort induces CYP3A4 [106] and therefore has the potential to decrease the plasma concentration of enzalutamide, a CYP3A4 substrate. Coadministration of St John’s Wort with enzalutamide should generally be avoided. Mushroom-derived supplements including lion’s mane, maitake, reishi, and turkey tail have been reported to have anticancer properties [107] and are very popular among patients with cancer. A recent series of Cancer Information Summaries on Prostate Cancer, Nutrition, and Dietary Supplements from the PDQ Integrative, Alternative, and Complementary Therapies Editorial Board [108] provided results on the interactions of foods and dietary supplements including Ca, green tea, lycopene, modified citrus pectin, pomegranate, selenium, soy, vitamin D, and vitamin E. Of these, there is evidence that green tea, modified citrus pectin, pomegranate, and soy are associated with a decreased risk of prostate cancer or beneficial effects for patients with prostate cancer [108]. There are no known drug interactions between enzalutamide and any of the following [9, 10]: lion’s mane, maitake, reishi, turkey tail, cordyceps, Ca 600 D (Ca/vitamin D), green tea, Theratrum Complete 50 Plus with lutein and lycopene, pectin, Emergen-C cranberry-pomegranate (multivitamin with minerals), selenium, soya lecithin, vitamin D2, vitamin E, or vitamin A. Turmeric and fish oil are also popular supplements that are not known to interact with enzalutamide [10]. These findings suggests that many popular supplements and vitamins may be safe to take together with enzalutamide, at least individually and at appropriate doses. However, the treating physician should always be made aware of all complementary and alternative medicines being taken by the patient so that their potential interactions with enzalutamide can be monitored.
5 Conclusions
Enzalutamide is a highly effective anti-androgen for the treatment of advanced prostate cancer [109]. However, it has potential risks of DDIs in certain situations. Enzalutamide interacts with key CYPs and transporters. It moderately induces CYP2C9 and CYP2C19 and strongly induces CYP3A4 [33]. Notably, CYP3A4 metabolizes approximately one third of drugs that are metabolized in the liver [110] and is the predominant source of enzalutamide DDIs. Therefore, by inducing CYP3A4, there is a potential for DDIs when enzalutamide is coadministered with a broad range of drugs that are CYP3A4 substrates including certain anticoagulants and antiplatelet agents, statins, Ca channel blockers, antiarryhythmic agents, and many others (Table 1). It is important to understand this and the other mechanisms of enzalutamide DDIs as they may result in a loss of efficacy when coadministering with other drugs or an increased risk of drug-related adverse effects. Fortunately, where DDIs pose challenges, it may be possible to rationally alter dosing, particularly with the integrated expertise of a multidisciplinary team of experts, and there are often alternative drugs that can be used that do not interact with enzalutamide or which pose minor or moderate risks.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer Stat Facts: Prostate Cancer 2022. Available from: https://seer.cancer.gov/statfacts/html/prost.html. Accessed 10 Apr 2023.
Chin HW, Kim J, Rasp G, Hristov B. Prostate cancer in seniors: part 1: epidemiology, pathology, and screening. Fed Pract. 2015;32(Suppl. 4):41S-44S.
Pettersson A, Robinson D, Garmo H, Holmberg L, Stattin P. Age at diagnosis and prostate cancer treatment and prognosis: a population-based cohort study. Ann Oncol. 2018;29(2):377–85. https://doi.org/10.1093/annonc/mdx742.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74. https://doi.org/10.1186/s12916-015-0322-7.
Astellas Inc. Highlights of prescribing information: XTANDI (enzalutamide) capsules, for oral use 2022. Available from: https://www.astellas.us/docs/us/12A005-ENZ-WPI.pdf. [Accessed 10 May 2023].
Benoist GE, van Oort IM, Smeenk S, Javad A, Somford DM, Burger DM, et al. Drug-drug interaction potential in men treated with enzalutamide: mind the gap. Br J Clin Pharmacol. 2018;84(1):122–9. https://doi.org/10.1111/bcp.13425.
European Medicines Agency. XTANDI (enzalutamide). Summary of product characteristics 2022. Available from: https://www.ema.europa.eu/en/documents/product-information/xtandi-epar-product-information_en.pdf. [Accessed 29 May 2022].
Drugs.com. Available from: https://www.drugs.com. [Accessed 5 Jan 2024].
Lexicomp. Drug interactions. Available from: http://online.lexi.com. [Accessed 5 Jan 2024].
Prescribers' Digital Reference. 2023. Available from: https://pdr.net/. [Accessed 5 Jan 2024].
Tsoukalas N, Brito-Dellan N, Font C, Butler T, Rojas-Hernandez CM, Butler T, et al. Complexity and clinical significance of drug-drug interactions (DDIs) in oncology: challenging issues in the care of patients regarding cancer-associated thrombosis (CAT). Support Care Cancer. 2022;30(10):8559–73. https://doi.org/10.1007/s00520-022-07235-8.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. https://doi.org/10.1056/NEJMoa0905561.
Bates ER, Lau WC, Angiolillo DJ. Clopidogrel-drug interactions. J Am Coll Cardiol. 2011;57(11):1251–63. https://doi.org/10.1016/j.jacc.2010.11.024.
Zhao M, Ma J, Li M, Zhang Y, Jiang B, Zhao X, et al. Cytochrome P450 enzymes and drug metabolism in humans. Int J Mol Sci. 2021;22(23). https://doi.org/10.3390/ijms222312808.
Eichelbaum M, Ingelman-Sundberg M, Evans WE. Pharmacogenomics and individualized drug therapy. Annu Rev Med. 2006;57:119–37. https://doi.org/10.1146/annurev.med.56.082103.104724.
Lauschke VM, Ingelman-Sundberg M. Prediction of drug response and adverse drug reactions: from twin studies to next generation sequencing. Eur J Pharm Sci. 2019;130:65–77. https://doi.org/10.1016/j.ejps.2019.01.024.
Bertz RJ, Granneman GR. Use of in vitro and in vivo data to estimate the likelihood of metabolic pharmacokinetic interactions. Clin Pharmacokinet. 1997;32(3):210–58. https://doi.org/10.2165/00003088-199732030-00004.
Evans WE, Relling MV. Pharmacogenomics: translating functional genomics into rational therapeutics. Science. 1999;286(5439):487–91. https://doi.org/10.1126/science.286.5439.487.
International Transporter Consortium. Membrane transporters in drug development. Nat Rev Drug Discov. 2010;9(3):215–36. https://doi.org/10.1038/nrd3028.
Chen Y, Tang Y, Guo C, Wang J, Boral D, Nie D. Nuclear receptors in the multidrug resistance through the regulation of drug-metabolizing enzymes and drug transporters. Biochem Pharmacol. 2012;83(8):1112–26. https://doi.org/10.1016/j.bcp.2012.01.030.
Geick A, Eichelbaum M, Burk O. Nuclear receptor response elements mediate induction of intestinal MDR1 by rifampin. J Biol Chem. 2001;276(18):14581–7. https://doi.org/10.1074/jbc.M010173200.
Synold TW, Dussault I, Forman BM. The orphan nuclear receptor SXR coordinately regulates drug metabolism and efflux. Nat Med. 2001;7(5):584–90. https://doi.org/10.1038/87912.
Willson TM, Kliewer SA. PXR, CAR and drug metabolism. Nat Rev Drug Discov. 2002;1(4):259–66. https://doi.org/10.1038/nrd753.
Armstrong AJ, Azad AA, Iguchi T, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, et al. Improved survival with enzalutamide in patients with metastatic hormone-sensitive prostate cancer. J Clin Oncol. 2022;40(15):1616–22. https://doi.org/10.1200/JCO.22.00193.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381(2):121–31. https://doi.org/10.1056/NEJMoa1903835.
Scher HI, Fizazi K, Saad F, Taplin M-E, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–97. https://doi.org/10.1056/NEJMoa1207506.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371(5):424–33. https://doi.org/10.1056/NEJMoa1405095.
Freedland SJ, de Almeida Luz M, De Giorgi U, Gleave M, Gotto GT, Pieczonka CM, et al. Improved outcomes with enzalutamide in biochemically recurrent prostate cancer. N Engl J Med. 2023;389(16):1453–65. https://doi.org/10.1056/NEJMoa2303974.
European Medicines Agency. Guideline on the investigation of drug interactions. 2012. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-investigation-drug-interactions-revision-1_en.pdf. Accessed 10 Apr 2023.
Scher HI, Beer TM, Higano CS, Anand A, Taplin M-E, Efstathiou E, et al. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet. 2010;375(9724):1437–46. https://doi.org/10.1016/S0140-6736(10)60172-9.
Gibbons JA, Ouatas T, Krauwinkel W, Ohtsu Y, van der Walt J-S, Beddo V, et al. Clinical pharmacokinetic studies of enzalutamide. Clin Pharmacokinet. 2015;54(10):1043–55. https://doi.org/10.1007/s40262-015-0271-5.
Gibbons JA, de Vries M, Krauwinkel W, Ohtsu Y, Noukens J, van der Walt J-S, et al. Pharmacokinetic drug interaction studies with enzalutamide. Clin Pharmacokinet. 2015;54(10):1057–69. https://doi.org/10.1007/s40262-015-0283-1.
US Food and Drug Administration. Center for Drug Evaluation and Research Application Number: 203415Orig1s000. Clin Pharmacol Biopharm Rev. 2012. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203415Orig1s000ClinPharmR.pdf. Accessed 28 Jun 2023.
Poondru S, Ghicavii V, Khosravan R, Manchandani P, Heo N, Moy S, et al. Effect of enzalutamide on PK of P-gp and BCRP substrates in cancer patients: CYP450 induction may not always predict overall effect on transporters. Clin Transl Sci. 2022;15(5):1131–42. https://doi.org/10.1111/cts.13229.
Albermann N, Schmitz-Winnenthal FH, Z’Graggen K, Volk C, Hoffmann MM, Haefeli WE, Weiss J. Expression of the drug transporters MDR1/ABCB1, MRP1/ABCC1, MRP2/ABCC2, BCRP/ABCG2, and PXR in peripheral blood mononuclear cells and their relationship with the expression in intestine and liver. Biochem Pharmacol. 2005;70(6):949–58. https://doi.org/10.1016/j.bcp.2005.06.018.
Sternberg CN, de Bono JS, Chi KN, Fizazi K, Mulders P, Cerbone L, et al. Improved outcomes in elderly patients with metastatic castration-resistant prostate cancer treated with the androgen receptor inhibitor enzalutamide: results from the phase III AFFIRM trial. Ann Oncol. 2014;25(2):429–34. https://doi.org/10.1093/annonc/mdt571.
Graff JN, Baciarello G, Armstrong AJ, Higano CS, Iversen P, Flaig TW, et al. Efficacy and safety of enzalutamide in patients 75 years or older with chemotherapy-naive metastatic castration-resistant prostate cancer: results from PREVAIL. Ann Oncol. 2016;27(2):286–94. https://doi.org/10.1093/annonc/mdv542.
Spratt DE, Shore N, Sartor O, Rathkopf D, Olivier K. Treating the patient and not just the cancer: therapeutic burden in prostate cancer. Prostate Cancer Prostatic Dis. 2021;24(3):647–61. https://doi.org/10.1038/s41391-021-00328-1.
Boujonnier F, Lemaitre F, Scailteux L-M. Pharmacokinetic interactions between abiraterone, apalutamide, darolutamide or enzalutamide and antithrombotic drugs: prediction of clinical events and review of pharmacological information. Cardiovasc Drugs Ther. 2023. https://doi.org/10.1007/s10557-023-07453-0.
Brodie MJ, Mintzer S, Pack AM, Gidal BE, Vecht CJ, Schmidt D. Enzyme induction with antiepileptic drugs: cause for concern? Epilepsia. 2013;54(1):11–27. https://doi.org/10.1111/j.1528-1167.2012.03671.x.
Shore ND, Morgans AK, El-Haddad G, Srinivas S, Abramowitz M. Addressing challenges and controversies in the management of prostate cancer with multidisciplinary teams. Target Oncol. 2022;17(6):709–25. https://doi.org/10.1007/s11523-022-00925-7.
Conde-Estevez D, Henriquez I, Munoz-Rodriguez J, Rodriguez-Vida A. Treatment of non-metastatic castration-resistant prostate cancer: facing age-related comorbidities and drug-drug interactions. Expert Opin Drug Metab Toxicol. 2022;18(9):601–13. https://doi.org/10.1080/17425255.2022.2122812.
Saad F, Shore ND. Relugolix: a novel androgen deprivation therapy for management of patients with advanced prostate cancer. Ther Adv Med Oncol. 2021;13:1758835921998586. https://doi.org/10.1177/1758835921998586.
Myovant Sciences Inc. Highlights of prescribing information: Orgovyx (relugolix) tablets, for oral use 2023. Available from: https://www.orgovyx.com/content/pdfs/orgovyx-prescribing-information.pdf. Accessed 10 Apr 2023.
Shore ND, Saad F, Cookson MS, George DJ, Saltzstein DR, Tutrone R, et al. Oral relugolix for androgen-deprivation therapy in advanced prostate cancer. N Engl J Med. 2020;382(23):2187–96. https://doi.org/10.1056/NEJMoa2004325.
George DJ, Saad F, Cookson MS, Saltzstein DR, Tutrone R, Bossi A, et al. Impact of concomitant prostate cancer medications on efficacy and safety of relugolix versus leuprolide in men with advanced prostate cancer. Clin Genitourin Cancer. 2023;21(3):383-92.e2. https://doi.org/10.1016/j.clgc.2023.03.009.
Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290–314. https://doi.org/10.1002/cncr.28509.
Morgans AK, Shore N, Cope D, McNatty A, Moslehi J, Gomella L, Sartor O. Androgen receptor inhibitor treatments: cardiovascular adverse events and comorbidity considerations in patients with non-metastatic prostate cancer. Urol Oncol. 2021;39(1):52–62. https://doi.org/10.1016/j.urolonc.2020.08.003.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0.
Mackman N, Bergmeier W, Stouffer GA, Weitz JI. Therapeutic strategies for thrombosis: new targets and approaches. Nat Rev Drug Discov. 2020;19(5):333–52. https://doi.org/10.1038/s41573-020-0061-0.
Bellia A, Della-Morte D, Di Daniele N, Lauro D. Drug interactions of direct oral anticoagulants in elderly patients with cardiometabolic diseases. Curr Res Pharmacol Drug Discov. 2021;2: 100029. https://doi.org/10.1016/j.crphar.2021.100029.
Otsuka Y, Poondru S, Bonate PL, Rose RH, Jamei M, Ushigome F, Minematsu T. Physiologically-based pharmacokinetic modeling to predict drug-drug interaction of enzalutamide with combined P-gp and CYP3A substrates. J Pharmacokinet Pharmacodyn. 2023;50:365–76. https://doi.org/10.1007/s10928-023-09867-7.
Boehringer Ingelheim Inc. Highlights of prescribing information: Pradaxa (dabigatran etexilate) capsules, for oral use 2021. Available from: https://content.boehringer-ingelheim.com/DAM/c669f898-0c4e-45a2-ba55-af1e011fdf63/pradaxa%20capsules-us-pi.pdf. Accessed 10 Apr 2023.
Bristol-Myers Squibb Inc. Highlights of prescribing information: coumadin (warfarin sodium) tablets, for oral use 2019. Available from: https://packageinserts.bms.com/pi/pi_coumadin.pdf. Accessed 10 Apr 2023.
CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996;348(9038):1329–39. https://doi.org/10.1016/s0140-6736(96)09457-3.
Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126–30. https://doi.org/10.1001/jama.293.17.2126.
van Werkum JW, Heestermans AA, Zomer AC, Kelder JC, Suttorp MJ, Rensing BJ, et al. Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol. 2009;53(16):1399–409. https://doi.org/10.1016/j.jacc.2008.12.055.
Schulz S, Schuster T, Mehilli J, Byrne RA, Ellert J, Massberg S, et al. Stent thrombosis after drug-eluting stent implantation: incidence, timing, and relation to discontinuation of clopidogrel therapy over a 4-year period. Eur Heart J. 2009;30(22):2714–21. https://doi.org/10.1093/eurheartj/ehp275.
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57. https://doi.org/10.1056/NEJMoa0904327.
Angiolillo DJ, Rollini F, Storey RF, Bhatt DL, James S, Schneider DJ, et al. International expert consensus on switching platelet P2Y(12) receptor-inhibiting therapies. Circulation. 2017;136(20):1955–75. https://doi.org/10.1161/CIRCULATIONAHA.117.031164.
Shah MB. Inhibition of CYP2C8 by acyl glucuronides of gemfibrozil and clopidogrel: pharmacological significance, progress and challenges. Biomolecules. 2022. https://doi.org/10.3390/biom12091218.
Sanofi Inc. Highlights of prescribing information: PLAVIX (clopidogrel tablets) for oral use 2022. Available from: https://products.sanofi.us/plavix/plavix.pdf. Accessed 10 Apr 2023.
AstraZeneca Inc. Highlights of prescribing information: BRILINTA (ticagrelor) tablets, for oral use. 2022. Available from: https://den8dhaj6zs0e.cloudfront.net/50fd68b9-106b-4550-b5d0-12b045f8b184/565ceafd-fbe3-4573-9c39-19280af566ec/565ceafd-fbe3-4573-9c39-19280af566ec_viewable_rendition__v.pdf. Accessed 10 Apr 2023.
Burger W, Chemnitius JM, Kneissl GD, Rucker G. Low-dose aspirin for secondary cardiovascular prevention: cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation: review and meta-analysis. J Intern Med. 2005;257(5):399–414. https://doi.org/10.1111/j.1365-2796.2005.01477.x.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124(22):2458–73. https://doi.org/10.1161/CIR.0b013e318235eb4d.
Maron DJ, Fazio S, Linton MF. Current perspectives on statins. Circulation. 2000;101(2):207–13. https://doi.org/10.1161/01.cir.101.2.207.
Parke-Davis Div of Pfizer Inc. Highlights of prescribing information: LIPITOR (atorvastin calcium) tablets, for oral use 2022. Available from: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=c6e131fe-e7df-4876-83f7-9156fc4e8228&type=display. Accessed 10 Apr 2023.
Organon Inc. Highlights of prescribing information: ZOCOR (simvastatin) tablets, for oral use 2022. Available from: https://www.organon.com/product/usa/pi_circulars/z/zocor/zocor_pi.pdf. Accessed 10 Apr 2023.
Lupin Inc. Lovastatin tablets USP 2021. Available from: https://www.lupin.com/US/wp-content/uploads/2020/12/pi-lovastatin-tabs-usp-1-2021.pdf. Accessed 10 Apr 2023.
Novartis Inc. Lescol XL (fluvastatin) package insert. 2017. Available from: https://www.novartis.com/sg-en/sites/novartis_sg/files/LESCOL%20%2080mg%20PI%20Decl2017.SIN_.pdf. Accessed 10 Apr 2023.
Lowe RN, Marrs JC, Saseen JJ. Patterns of serum laboratory monitoring for safety and efficacy in patients on chronic statin therapy. Ther Adv Drug Saf. 2013;4(1):9–17. https://doi.org/10.1177/2042098612474293.
Schachter M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundam Clin Pharmacol. 2005;19(1):117–25. https://doi.org/10.1111/j.1472-8206.2004.00299.x.
Jones PH, Davidson MH, Stein EA, Bays HE, McKenney JM, Miller E, et al. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR* Trial). Am J Cardiol. 2003;92(2):152–60. https://doi.org/10.1016/s0002-9149(03)00530-7.
Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, Sanchez E. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. J Am Coll Cardiol. 2014;63(12):1230–8. https://doi.org/10.1016/j.jacc.2013.11.007.
Flockhart DA, Tanus-Santos JE. Implications of cytochrome P450 interactions when prescribing medication for hypertension. Arch Intern Med. 2002;162(4):405–12. https://doi.org/10.1001/archinte.162.4.405.
Pfizer Laboratories Div Pfizer Inc. Highlights of prescribing information: NORVASC (amlodipine besylate) tablets for oral administration 2019. Available from: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=abd6a2ca-40c2-485c-bc53-db1c652505ed&type=display. Accessed 10 Apr 2023.
Brown NJ, Vaughan DE. Angiotensin-converting enzyme inhibitors. Circulation. 1998;97(14):1411–20. https://doi.org/10.1161/01.cir.97.14.1411.
Leonetti G, Egan CG. Use of carvedilol in hypertension: an update. Vasc Health Risk Manag. 2012;8:307–22. https://doi.org/10.2147/VHRM.S31578.
Lei M, Wu L, Terrar DA, Huang CL. Modernized classification of cardiac antiarrhythmic drugs. Circulation. 2018;138(17):1879–96. https://doi.org/10.1161/CIRCULATIONAHA.118.035455.
Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. Proc (Bayl Univ Med Cent). 2003;16(1):123–6. https://doi.org/10.1080/08998280.2003.11927893.
Szema AM, Dang S, Li JC. Emerging novel therapies for heart failure. Clin Med Insights Cardiol. 2015;9(Suppl. 2):57–64. https://doi.org/10.4137/CMC.S29735.
Zhang M, Zou Y, Li Y, Wang H, Sun W, Liu B. The history and mystery of sacubitril/valsartan: from clinical trial to the real world. Front Cardiovasc Med. 2023;10:1102521. https://doi.org/10.3389/fcvm.2023.1102521.
Cowie MR, Fisher M. SGLT2 inhibitors: mechanisms of cardiovascular benefit beyond glycaemic control. Nat Rev Cardiol. 2020;17(12):761–72. https://doi.org/10.1038/s41569-020-0406-8.
Iqbal J, Parviz Y, Pitt B, Newell-Price J, Al-Mohammad A, Zannad F. Selection of a mineralocorticoid receptor antagonist for patients with hypertension or heart failure. Eur J Heart Fail. 2014;16(2):143–50. https://doi.org/10.1111/ejhf.31.
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. https://doi.org/10.1038/nrdp.2015.19.
Yang F, Liu L, Chen L, Liu M, Liu F, Xiong Y, et al. OATP1B3 (699G>A) and CYP2C9*2, *3 significantly influenced the transport and metabolism of glibenclamide and glipizide. Sci Rep. 2018;8(1):18063. https://doi.org/10.1038/s41598-018-36212-7.
Dave DJ. Saxagliptin: A dipeptidyl peptidase-4 inhibitor in the treatment of type 2 diabetes mellitus. J Pharmacol Pharmacother. 2011;2(4):230–5. https://doi.org/10.4103/0976-500X.85934.
Kashiwagi A, Maegawa H. Metabolic and hemodynamic effects of sodium-dependent glucose cotransporter 2 inhibitors on cardio-renal protection in the treatment of patients with type 2 diabetes mellitus. J Diabetes Investig. 2017;8(4):416–27. https://doi.org/10.1111/jdi.12644.
Rao A, Cohen HJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr. 2004;32:150–7. https://doi.org/10.1093/jncimonographs/lgh031.
Edinoff AN, Akuly HA, Hanna TA, Ochoa CO, Patti SJ, Ghaffar YA, et al. Selective serotonin reuptake inhibitors and adverse effects: a narrative review. Neurol Int. 2021;13(3):387–401. https://doi.org/10.3390/neurolint13030038.
Isbister GK, Bowe SJ, Dawson A, Whyte IM. Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose. J Toxicol Clin Toxicol. 2004;42(3):277–85. https://doi.org/10.1081/clt-120037428.
van Haelst IM, van Klei WA, Doodeman HJ, Warnier MJ, De Bruin ML, Kalkman CJ, Egberts TC. QT interval prolongation in users of selective serotonin reuptake inhibitors in an elderly surgical population: a cross-sectional study. J Clin Psychiatry. 2014;75(1):15–21. https://doi.org/10.4088/JCP.13m08397.
Raskin J, Wiltse CG, Dinkel JJ, Walker DJ, Desaiah D, Katona C. Safety and tolerability of duloxetine at 60 mg once daily in elderly patients with major depressive disorder. J Clin Psychopharmacol. 2008;28(1):32–8. https://doi.org/10.1097/jcp.0b013e318160738e.
Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline Amendment 2019. J Urol. 2019;202(3):558–63. https://doi.org/10.1097/JU.0000000000000309.
Welk B, McClure JA. The impact of anticholinergic use for overactive bladder on cognitive changes in adults with normal cognition, mild cognitive impairment, or dementia. Eur Urol Open Sci. 2022;46:22–9. https://doi.org/10.1016/j.euros.2022.10.008.
Guay DR. Clinical pharmacokinetics of drugs used to treat urge incontinence. Clin Pharmacokinet. 2003;42(14):1243–85. https://doi.org/10.2165/00003088-200342140-00004.
Roehrborn CG, Siami P, Barkin J, Damiao R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57(1):123–31. https://doi.org/10.1016/j.eururo.2009.09.035.
Smith HS. Opioid metabolism. Mayo Clin Proc. 2009;84(7):613–24. https://doi.org/10.1016/S0025-6196(11)60750-7.
Detert Oude Weme SEH, Vervenne WL, Imhoz ALT, Cremers RGHM, van Berlo-van de Laar IFR, Jansman FGA, et al. Assessment of the pharmacokinetic interaction of enzalutamide with oxycodone in men with prostate cancer: the ENZYME study. Ann Oncol. 2022;33(Suppl._7):S713-42.
Strand DS, Kim D, Peura DA. 25 Years of proton pump inhibitors: a comprehensive review. Gut Liver. 2017;11(1):27–37. https://doi.org/10.5009/gnl15502.
Covis Pharma Inc. Highlights of prescribing infomration: Prilosec (omeprazole magnesium) for delayed-release oral suspension 2022. Available from: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=b6761f84-53ac-4745-a8c8-1e5427d7e179&type=display. Accessed 30 Apr 2023.
Katsuki H, Yagi H, Arimori K, Nakamura C, Nakano M, Katafuchi S, et al. Determination of R(+)- and S(-)-lansoprazole using chiral stationary-phase liquid chromatography and their enantioselective pharmacokinetics in humans. Pharm Res. 1996;13(4):611–5. https://doi.org/10.1023/a:1016062508580.
Shihab F, Christians U, Smith L, Wellen JR, Kaplan B. Focus on mTOR inhibitors and tacrolimus in renal transplantation: pharmacokinetics, exposure-response relationships, and clinical outcomes. Transpl Immunol. 2014;31(1):22–32. https://doi.org/10.1016/j.trim.2014.05.002.
FitzGerald JD, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles AM, et al. 2020 American College of Rheumatology guideline for the management of gout. Arthritis Care Res (Hoboken). 2020;72(6):744–60. https://doi.org/10.1002/acr.24180.
Sparreboom A, Cox MC, Acharya MR, Figg WD. Herbal remedies in the United States: potential adverse interactions with anticancer agents. J Clin Oncol. 2004;22(12):2489–503. https://doi.org/10.1200/JCO.2004.08.182.
Venturella G, Ferraro V, Cirlincione F, Gargano ML. Medicinal mushrooms: bioactive compounds, use, and clinical trials. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22020634.
National Cancer Institute. Prostate cancer, nutrition, and dietary supplements (PDQ) - health professional version. Available from: https://www.cancer.gov/about-cancer/treatment/cam/hp/prostate-supplements-pdq. Accessed 10 Apr 2023.
Sternberg CN. Enzalutamide, an oral androgen receptor inhibitor for treatment of castration-resistant prostate cancer. Future Oncol. 2019;15(13):1437–57. https://doi.org/10.2217/fon-2018-0940.
Kasichayanula S, Boulton DW, Luo WL, Rodrigues AD, Yang Z, Goodenough A, et al. Validation of 4beta-hydroxycholesterol and evaluation of other endogenous biomarkers for the assessment of CYP3A activity in healthy subjects. Br J Clin Pharmacol. 2014;78(5):1122–34. https://doi.org/10.1111/bcp.12425.
Acknowledgments
Raj Patel, PharmD (Pfizer Inc.) contributed to the conception and development of the manuscript. Medical writing and editorial support were provided by Peter Gray, PhD, and Rosie Henderson, MSc, both of Onyx (a division of Prime, London, UK), and funded by Pfizer Inc. and Astellas Pharma, Inc., the co-developers of enzalutamide. Pfizer and Astellas Pharma were involved in the study design, collection, analysis and interpretation of data, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding was provided by Pfizer Inc. and Astellas Pharma, Inc.
Conflicts of Interest/Competing Interests
Brandon Lennep has received consulting fees from Pfizer Inc. Jesse Mack is an employee of Astellas Pharma Inc. and was a consultant for Pfizer prior to joining Astellas Pharma Inc. Srinivasu Poondru is an employee of Astellas Pharma Inc. Brooke Looney receives research support from AstraZeneca Inc. and Pfizer Inc. and has served as a speaker for AstraZeneca Inc. Judeth Bianco is an employee of Pfizer Inc. Alicia Morgans has received consulting fees from Astellas Pharma Inc., AAA Pharma Inc., AstraZeneca Pharma LP, Bayer HealthCare Pharma LLC, Dendreon Pharma LLC, Janssen Pharma LLC, Exelixis Inc., Myovant Sciences, Inc., Merck & Co. Inc., Novartis AG, Lantheus, Telix Pharma Limited, Sanofi S.A., and Pfizer Inc., research fees from Bayer HealthCare Pharma LLC, Myovant Sciences Inc., and Pfizer Inc., and travel support from Telix Pharma Limited and Sanofi S.A. Elizabeth Hood and Monique Williams have no financial interests to declare.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors’ Contributions
BL, AM, and JB contributed to the conception of the study. All authors contributed to the design and interpretation of the results. All authors contributed to the drafting of the paper and/or to its revision or critical review. All authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lennep, B.W., Mack, J., Poondru, S. et al. Enzalutamide: Understanding and Managing Drug Interactions to Improve Patient Safety and Drug Efficacy. Drug Saf 47, 617–641 (2024). https://doi.org/10.1007/s40264-024-01415-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-024-01415-7